More Pregnant Women in the U.S. Are Delaying Prenatal Care — CDC Warns of a Growing Health Risk
Across the United States, a troubling trend has surfaced that may affect the health of thousands of mothers and their babies: fewer pregnant women are getting medical care early in pregnancy, according to a new report from the Centers for Disease Control and Prevention (CDC). Early prenatal care — usually begun in the first three months — gives doctors a chance to catch and treat problems before they worsen. But recent data shows that many expectant mothers are waiting longer to seek help, and in some cases getting little or no care at all before delivery.
This story isn’t just about numbers — it’s about real families, real fears, and barriers in a healthcare system that for too many Americans feels out of reach.
The Findings: A Shift in When Care Begins
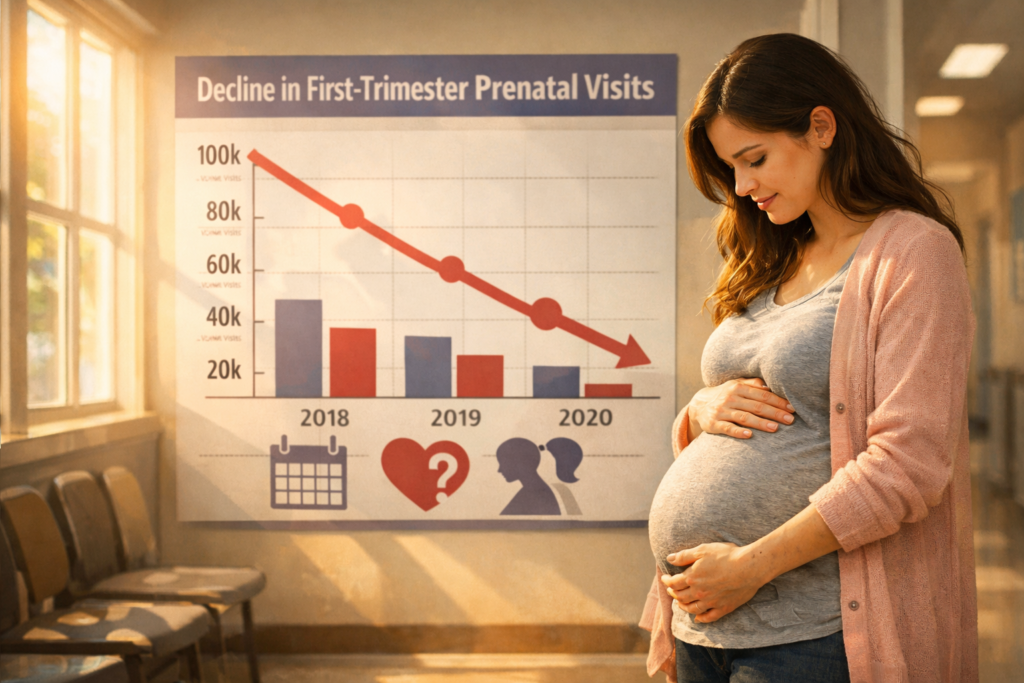
The CDC’s latest national prenatal care timing report shows a clear change in how soon women are accessing prenatal services:
- In 2021, 78.3% of pregnant women began prenatal care in the first trimester.
- By 2024, that figure fell to 75.5%.
- Meanwhile, more women started care in the second trimester (up from 15.4% to 17.3%).
- And the share of women getting late care or no care at all rose from 6.3% to 7.3% over the same period.
Those numbers matter. First-trimester visits help healthcare providers diagnose and manage conditions like high blood pressure, diabetes, and other complications that could endanger mother or baby if left undetected. Delayed care can mean missed opportunities to support healthier pregnancies and safer births.
A Personal and Public Health Concern
Doctors warn that when prenatal care begins later or not at all, it can seriously jeopardize both maternal and fetal well-being. Early visits typically include essential checks such as:
- Blood pressure screening
- Blood and urine tests
- Ultrasound imaging
- Nutritional and health guidance
OB-GYNs like Dr. Clayton Alfonso tell reporters that starting care early gives providers the best chance to spot complications before they become crises — a safeguard families often take for granted.
Delaying care might not just be a personal choice — for many, it’s about access, cost and location. In rural and underserved communities, obstetric providers are disappearing as hospitals shut labor and delivery units. A 2024 March of Dimes study found that more than 35% of U.S. counties lack basic maternal care services, meaning some families must travel long distances for appointments.
Disparities: Who Is Most Affected?
The report’s findings also highlight troubling disparities among mothers of different racial and ethnic backgrounds:
- Black mothers saw the largest drop in first-trimester care — from 69.7% in 2021 to 65.1% in 2024.
- Hispanic mothers and other minority groups also experienced declines in early care and increases in late or no care.
These differences matter deeply because maternal mortality and serious pregnancy complications are already higher among Black women and other marginalized groups — a longstanding issue in U.S. maternal health that experts and advocates have been raising for years.
When care is delayed, there’s less time to prevent or manage risks. Conditions like high blood pressure during pregnancy, which can damage organs or trigger dangerous outcomes if untreated, are more common than many realize — and doctors rely on early visits to catch them.
Why Are Women Waiting?
The CDC report didn’t drill into why more women are seeking care later, but public health experts point to a handful of likely causes:
Healthcare Access Gaps
- Maternity care deserts — where no prenatal providers exist
- Clinic closures and fewer obstetric practices in rural areas and smaller cities
- Lack of transportation or long travel distances
Financial Barriers
- Insurance hurdles, especially for women on Medicaid
- Cost uncertainty even with coverage
Post-Roe Reality and Provider Shortages
- Restrictions on abortion care have contributed to some doctors leaving states with strict laws, creating shortages in maternity care providers
- As a result, many expectant mothers struggle to find timely care appointments
Experts worry that if current trends continue, the impacts on maternal morbidity and mortality could grow more severe each year.
Real Lives Behind the Numbers
Consider the experience of Sarah, a 28-year-old mom-to-be living in a rural county with no OB-GYN clinic within 50 miles. She knew her pregnancy was progressing, but securing transportation — and taking time off work — meant waiting until she was 20 weeks along before she could see a provider. “It felt like every week that passed was a risk I couldn’t afford to take,” she told a local reporter. Stories like Sarah’s are becoming all too familiar as access tightens and pressures mount on expectant families.
And it doesn’t stop with physical health. Many families describe emotional stress, anxiety and fear — wondering whether they are doing the right thing for their babies and themselves when staging prenatal visits feels like a logistical puzzle.
A Call to Action for Families and Providers
Healthcare providers emphasize that early prenatal care remains one of the strongest predictors of healthier pregnancies and births. When women connect with providers early, they are more likely to receive:
- Vaccinations and screenings
- Early detection of conditions like gestational diabetes
- Guidance on nutrition, exercise and risk avoidance
- Emotional support and resources for a healthy pregnancy
Medical professionals are urging policymakers, insurers and community organizations to bridge gaps in care — especially in communities with growing rates of late or no prenatal care — to ensure that every mom and baby has the best possible start.







